Venous Sinus Stenting is a minimally invasive procedure for the treatment of Venous Sinus Stenosis. As the name implies, it involves placement of a metallic mesh in the shape of a tube (“stent”) in the area of narrowed vein in order to expand the vein and resolve the narrowing.
This procedure was first performed overseas (Australia, UK, France). In 2012 I started the first prospective clinical in the United States which showed significant benefit for patients with Idiopathic Intracranial Hypertension treated with venous sinus stenting.
This was followed by a second clinical trial which I also conducted, looking into the effectiveness of venous sinus stenting in patients with pulsatile tinnitus. The results of this study are quite promising and will be published soon in the medical literature.
Overall, I have performed more than 200 venous sinus stenting procedures with excellent results. I have treated children as young as 2 years of age and adults in their 60s.
Procedure
The procedure is done via a small incision in a vein in the upper part of the leg or the arm. During the last 6 months, I have been performing the procedure via the upper arm and we have published our experience. The technique is called SAVeS “Single Arm Access Venous Sinus Stenting (SAVeS)” and the advantage compared to the traditional approach through the leg, is that by going through the arm we avoid advancing catheters through the heart, we allow the patients to sit up or get up and walk early after the procedure, and we also avoid x-ray over the pelvis.
The venous sinus stenting procedure has two parts:
Catheter Venogram and Manometry
This is the initial part of the procedure during which a small catheter (size similar to a very thin spaghetti) is advanced via the arm or leg vein into the venous sinus in the head. By injecting contrast and measuring the pressures in the veins, we can confirm that the narrowing is severe enough to warrant stenting.
This part is performed with the patient awake as the measurements are more accurate if the patient is not under general anesthesia.
Stent placement
The second part of the procedure is the placement of the stent using the same route as the first step. Even though I did perform this part with patients awake, in general I prefer general anesthesia for this part as it can be uncomfortable for the awake patient.
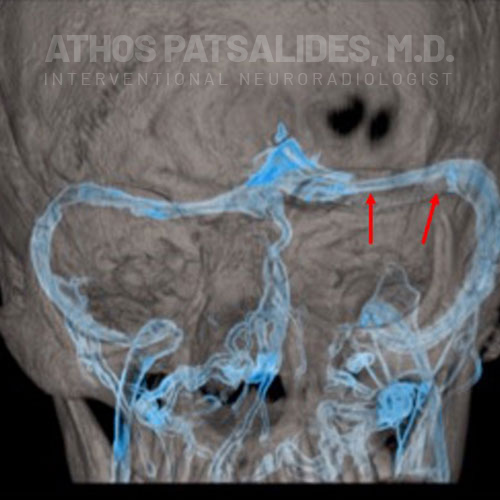
Pre Stent
This is an image showing venous sinuses in blue. Area of stenosis is demonstrated with red arrows.
Post Stent
A stent is shown in red.

Blood Thinners
Any procedure that involves placement of a stent requires the use of blood thinners. There is no universal way of which blood thinners to give and for how long.
The protocol I generally use is the following:
- Starting 5-7 days before the stenting procedure: Aspirin and Plavix
- From the stenting procedure until 1 month after: Aspirin and Plavix
- From 1 month to 1 year after the stenting procedure: Aspirin only
Please note that there can be changes according to the individual patient’s needs.
Indications for Venous Sinus Stenting
Idiopathic Intracranial Hypertension
The main indication of venous sinus stenting is to treat patients with Idiopathic Intracranial Hypertension (IIH). As we discuss in detail in the relevant section, venous sinus stenting can be used as a treatment option for patients who fail or do not tolerate medical therapy. Clinical research at Cornell and other institutions world-wide has shown that venous sinus is an effective treatment for IIH. Careful selection of patients is important as the procedure will not be effective for every patient.
-
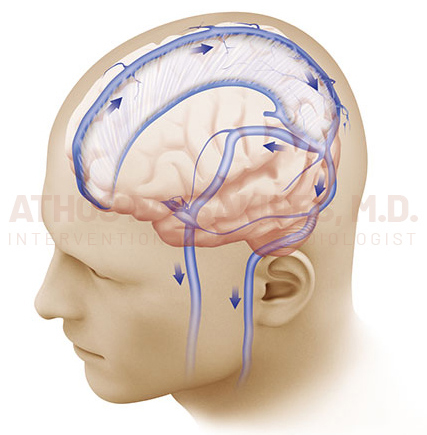
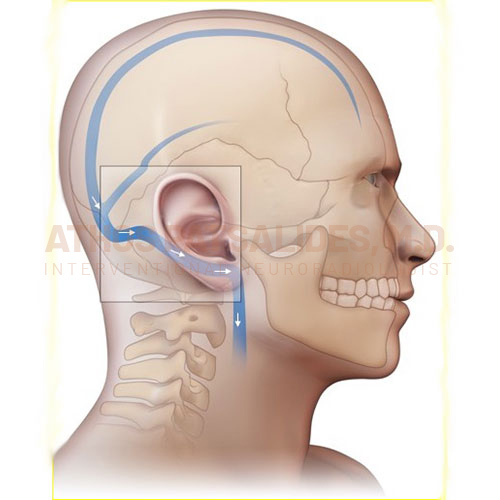
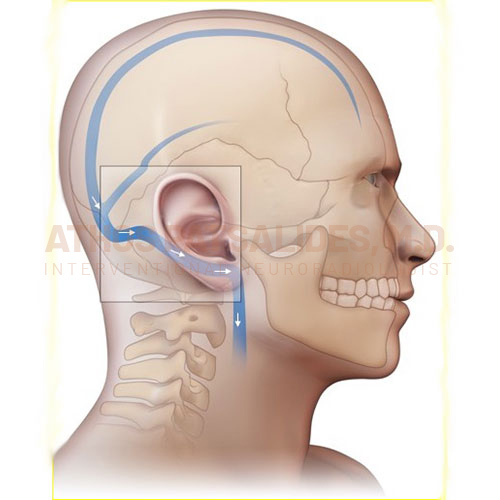
The illustration shows normal veins draining blood from the brain towards the neck (blue arrows)
-
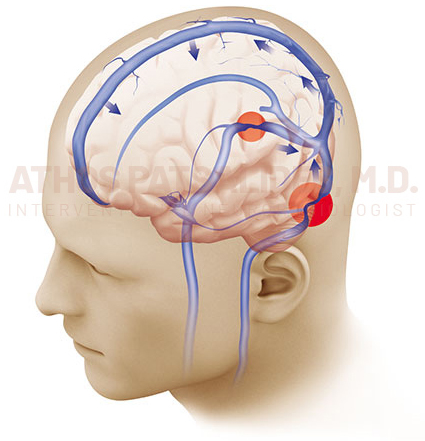
The illustration shows venous sinus stenosis (red circles). As a result of the narrowed veins, blood flow from the brain to the neck is compromised, leading to build of pressure in the veins (blue arrows) and subsequently increased intracranial pressure and IIH.
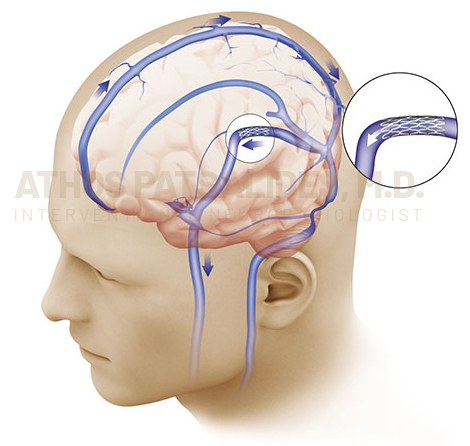
The venous sinus narrowing has been treated with placement of a stent (circle). After stenting, the blood flow from the brain to the neck is restored (blue arrows), leading to normalized intracranial pressure and improvement of the symptoms of IIH.
Pulsatile Tinnitus
We now know that some patients with pulsatile tinnitus have venous sinus stenosis as the underlying cause. This is often associated with expansion of the vein past the stenosis, a condition called venous diverticulum (or venous aneurysm). The combination of narrowing and expansion of the vein, causes turbulent flow adjacent to the ear, resulting in pulsatile tinnitus.
-
The illustration shows NORMAL venous sinuses in proximity to the ear. Normal blood flow is from the head towards the neck (white arrows).
-
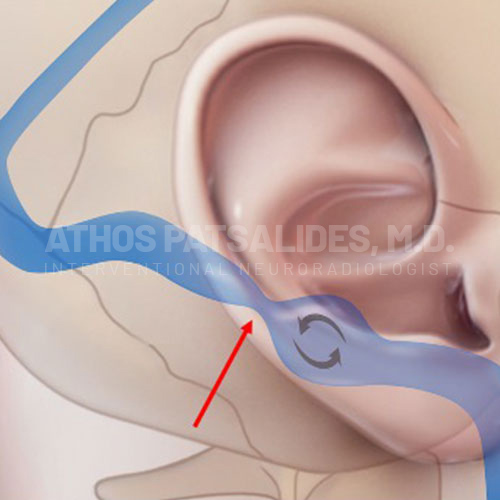
The illustration shows NARROWED venous sinuses (red arrow) in proximity to the ear. Because of the stenosis there is turbulent blood flow causing pulsatile tinnitus (curved arrows).
-
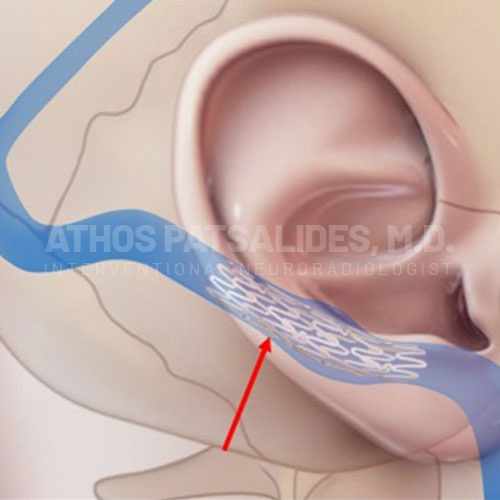
Stenting alleviates the stenosis, restores normal blood flow and eliminates pulsatile tinnitus.
Sometimes the expansion of the vein past the stenosis can be quite significant leading to formation of a large venous diverticulum or aneurysm. Please note that a venous diverticulum or aneurysm is very different from an arterial brain aneurysm. Arterial aneurysms are associated with brain bleed and stroke, whereas a venous aneurysm is not associated with brain bleed and stroke.
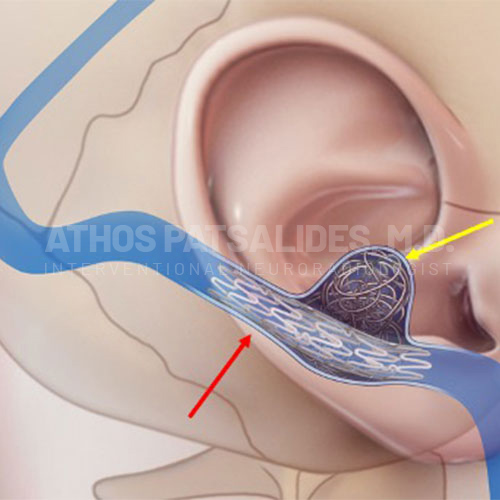
For patients with a large venous diverticulum, in addition to the stent, placement of coils (soft platinum wires) is necessary in order to stop blood flow within the venous diverticulum and help eliminate the pulsatile tinnitus.
-
The illustration shows NORMAL venous sinuses in proximity to the ear. Normal blood flow is from the head towards the neck (white arrows).
-
The illustration shows NARROWED venous sinuses (red arrow) in proximity to the ear. In addition, there is a large venous aneurysm, diverticulum (yellow arrow). Because of the stenosis and the large diverticulum, there is turbulent blood flow causing pulsatile tinnitus (curved arrows).

-
A combination of stenting (red arrow) and coiling (yellow arrow) alleviates the stenosis and occludes the venous diverticulum, restores normal blood flow and eliminates pulsatile tinnitus.
What to Expect?
Patients are typically admitted overnight but as the technique continues to improve (the “SAVeS” technique for example) I anticipate that many patients will be discharged on the same day.
One third of patients experience moderate to severe headache after the stenting procedure. This happens because there are nerves around the veins and by opening the narrowing there is expected irritation of these nerves. If the pain is moderate or severe, it’s always much improved within 24 hours. Patients should also expect to experience pain and discomfort when they cough or sneeze, sometimes for 2 weeks.
The patients should also anticipate easy bruising for the month after the procedure due to taking two blood thinners (Aspirin and Plavix).
